We’ve heard it before and yet it may still be hard to believe: Our zip code determines our health more than our genetic code. Why is this important for business owners? Because poor health impacts us all through greater costs for businesses and higher taxes. Specifically, businesses are impacted by:
- Healthcare expenses are a direct cost for employers, whether through employer- provided insurance or public options supported by taxes.
- Higher rates of disability due to illness and injury generate higher insurance rates.
- Absences for illnesses and doctor’s appointments plus presenteeism (working whilesick) affect productivity.
- Poor health can lead to higher rates of employee turnover, causing greater costs forrecruitment and training.On a national level, this leads to what is known as the U.S. Healthcare Disadvantage and impacts our competitiveness globally. Chronic illnesses and injuries in the workforce cost U.S. employers more than half a trillion dollars (+$500,000,000) and 1.5 billion days in lost productivity each year. That’s a cost of almost $4,000 per employee on average!
What can be done? Many communities are looking for solutions ‘upstream’—before the illnesses and injuries occur. This is cost- effective because every $1 spent on prevention saves $5.60 on health spending “downstream.”“Most of the time we’re busy paying for illness and injuries on an individual basis ‘downstream’—or after they’ve occurred,” explained Amber Wier, previously a small business advisor for the North Coast Small Business Development Center and currently the Project Director of the California Health Collaborative’s NorCal 4 Health project. “This can be really costly for everyone, but specifically forbusinesses through direct and indirect costs, such as productivity loss, insurance rates and higher taxes.”
As it turns out, most poor health outcomes are preventable and those that contribute to over 50% of deaths in California are due to personal behaviors around food, activity, and tobacco use. This phenomenon can be summed up by what is known as the 3-4-50 framework:

How do these behaviors translate in Lake County?
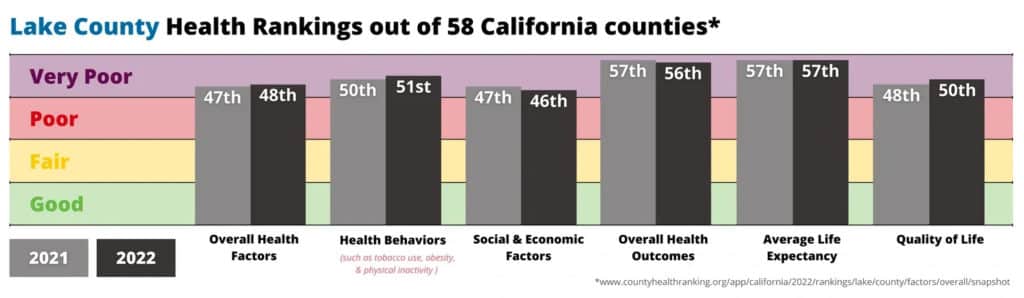
In the graphic below we can see that Lake County is behind in categories:
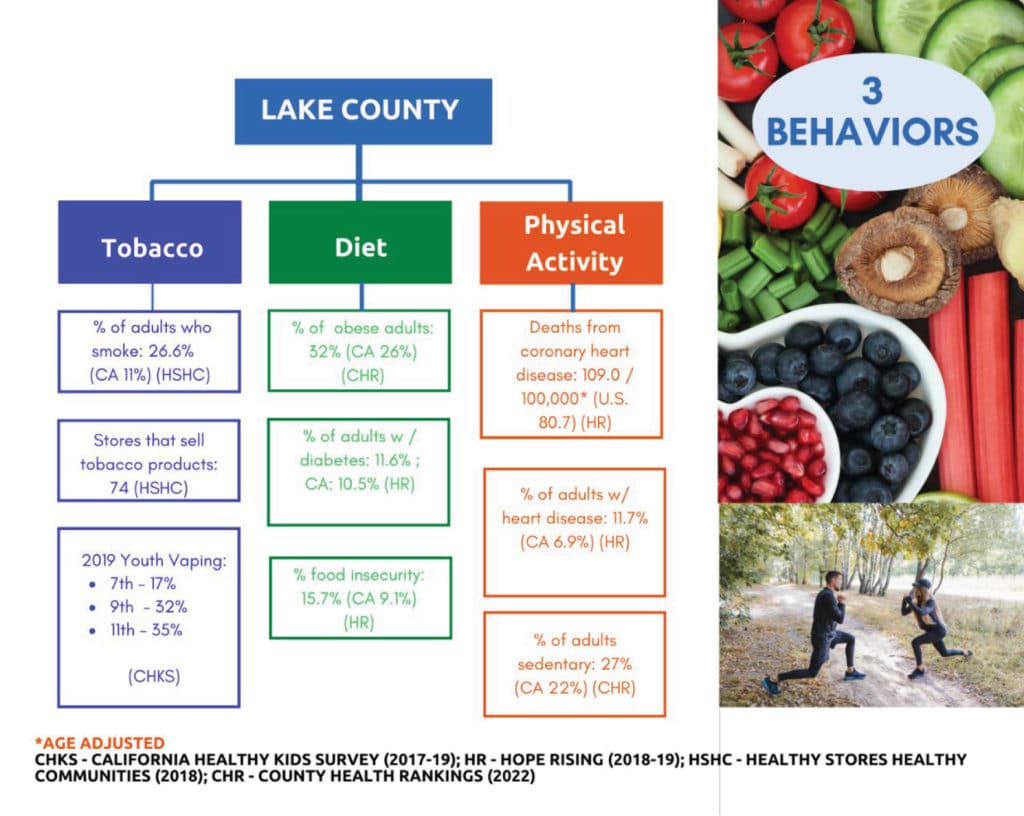
Below we can see Lake County residents suffer from higher rates of tobacco/nicotine use, heart disease, and food insecurity, which contribute to the county’s “very poor” health rankings:
Promising Community-level Solutions
While we bring to light the three behavior areas that contribute to the four diseases that account for more than 50% of the deaths, addressing those behaviors on an individual level is just one point of opportunity for change. Remember the zip code determinant above? Health starts long before illness. As we now know, in America, 80-90% of health outcomes are the result of conditions in communities.¹
Additionally, the same vital conditions that shape health are the very features that attract and retain talented workers, loyal customers, tourists and prosperous businesses to a community. Some of these features include safe parks and green spaces, quality, affordable housing and public transportation, access to healthy foods, access to childcare and early childhood education, quality schools, and feelings of civic pride and responsibility.
As it happens, in America, 80-90% of health outcomes are the result of conditions in communities.¹ Additionally, the same vital conditions that shape health are the very features that attract and retain talented workers, loyal customers, tourists and prosperous businesses to a community.
Policies and planning decisions that build in healthier choices, like bike lanes, smoke-free outdoor spaces, smoke-free shared-wall housing (also known as multi-unit housing), and increasing access in neighborhoods for most things needed for daily living, like healthy food and household items, lead to better health outcomes naturally.”
Further, for many rural communities that rely on tourism dollars, reducing harmful tobacco consumption, secondhand smoke, and tobacco product waste helps attract tourists, especially those from urban areas who expect a tobacco-free environment.
“What we’re noticing is that communities that put specific features in place in their built environment have created natural and effortless conditions for not only better health for everyone,” concluded Wier. “but, also for better local economies. In other words, how we shape our community, in turn, shapes us.”
“We know it’s hard to think about when we’re busy working our business and assisting people in immediate need,” acknowledged Wier, “but spending a little more time addressing why they are in need, improving community conditions, and tackling the problem before it happens will ultimately save us time, money and provide a better quality of life for the long run.”
She continued, “Community health is part of business health and local business owners can have influence. They can use their voice to let elected officials know they want to create a more viable economic future through upstream prevention and planning. Speak up at public meetings. Email or call their representatives. Small businesses can influence community health and prosperity by encouraging government and local planning projects to incorporate upstream thinking and design.”
Wier invites business owners to learn more at their website www.NorCal4Health.org and looks to the Community Health and Economic Prosperity (CHEP) initiative enacted by previous Surgeon General, Jerome Adams, for inspiration: “Health and the economy are inextricably linked and both most thrive if either is to be strong.”
NorCal 4 Health is a project of the California Health Collaborative serving Lake, Mendocino, Humboldt, and Del Norte Counties. It provides education and resources on community-level solutions to elevate health and economic prosperity. The project is funded by the California Department of Public Health and works alongside local residents and organizations. Learn more at www.NorCal4Health.org
¹ Hood, C. M., Gennuso, K. P., Swain, G. R., & Catlin, B. B. (2016). County health rankings: Relationships between determinant factors and health outcomes. American Journal of Preventive Medicine, 50(2), 129–135. Retrieved from: https://www.hhs.gov/sites/default/files/chep-sgr-causes-health-disadvantage-fs3.pdf.
